By 2026, hospitals planning to build clinical documentation software are operating under increasing administrative pressure, clinician burnout, and rising expectations for care quality and regulatory compliance. Documentation has become a core operational constraint, with direct impact on reimbursement timelines, audit exposure, clinician capacity, and care consistency.
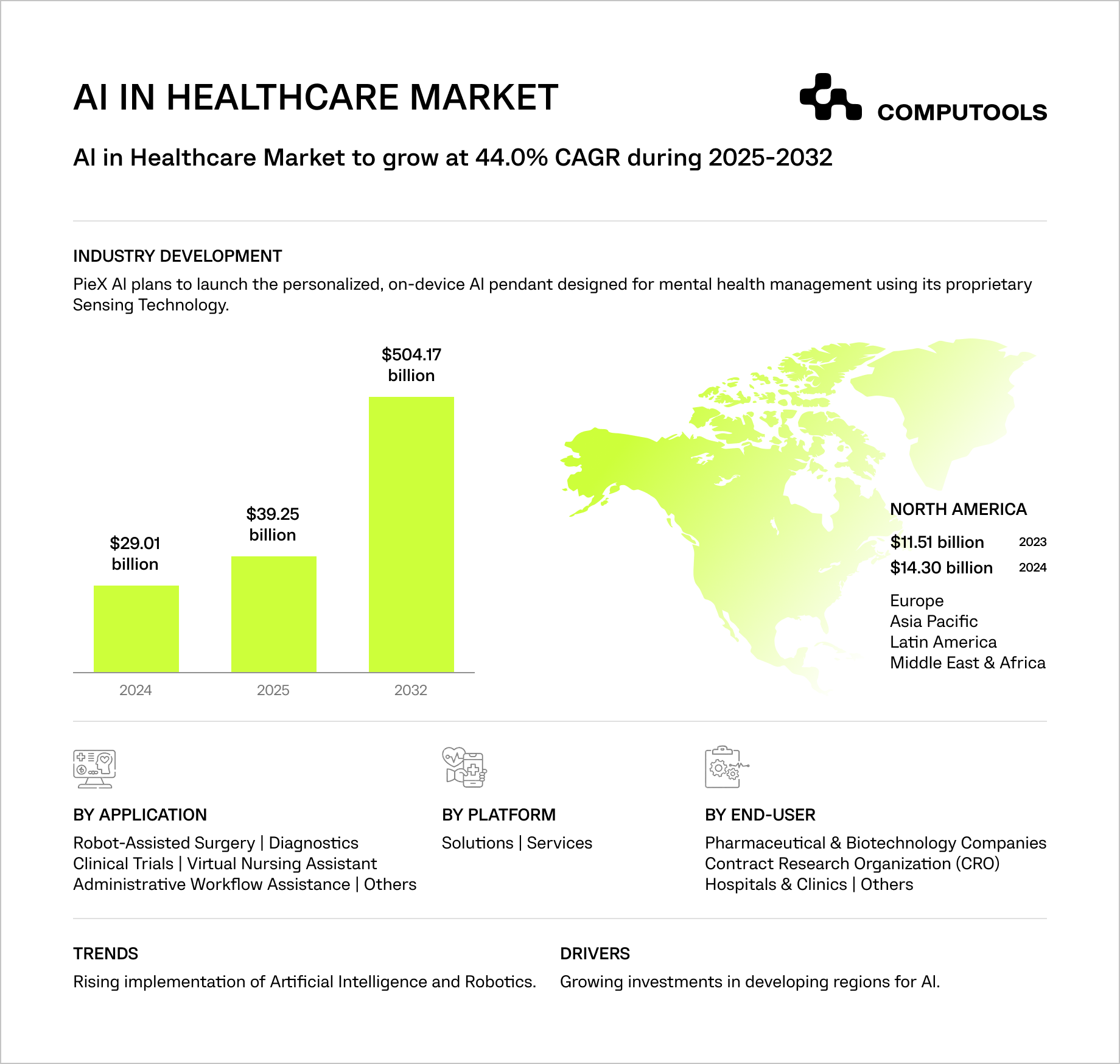
This shift is reflected in market dynamics. The global AI in healthcare market was valued at $39.34 billion in 2025 and is expected to grow from $56.01 billion in 2026 to over $1 trillion by 2034, with an almost 44% CAGR. North America alone accounted for 44.5% of the market, highlighting how rapidly healthcare providers are investing in AI solutions that deliver measurable operational and financial impact.
AI adoption in healthcare has moved beyond pilots. Over 85% of healthcare organizations already use AI in some capacity, while more than 20% have deployed domain-specific solutions in production.
Hospitals using AI-driven documentation report up to 65% less time spent on paperwork and over 40% improvements in diagnostic accuracy, directly impacting physician capacity, revenue cycles, and care consistency.
As patient volumes grow, traditional hospital documentation software struggles to scale without introducing data fragmentation and workflow friction.
Hospital executives and IT leaders face an architectural challenge: tight coupling of EHRs, documentation, and coding creates brittleness and limits AI adoption. By 2026, the focus shifts from automating documentation to building secure, scalable, and reliable AI that integrates with workflows without increasing risk.
How Computools implemented an AI-driven clinical documentation system in practice
Many healthcare organizations struggle with the same structural issue: clinical data is generated across multiple systems, while documentation and analysis remain fragmented and difficult to scale. As patient volumes increase, this disconnect slows clinical workflows, limits data-driven decision-making, and increases the risk of errors.
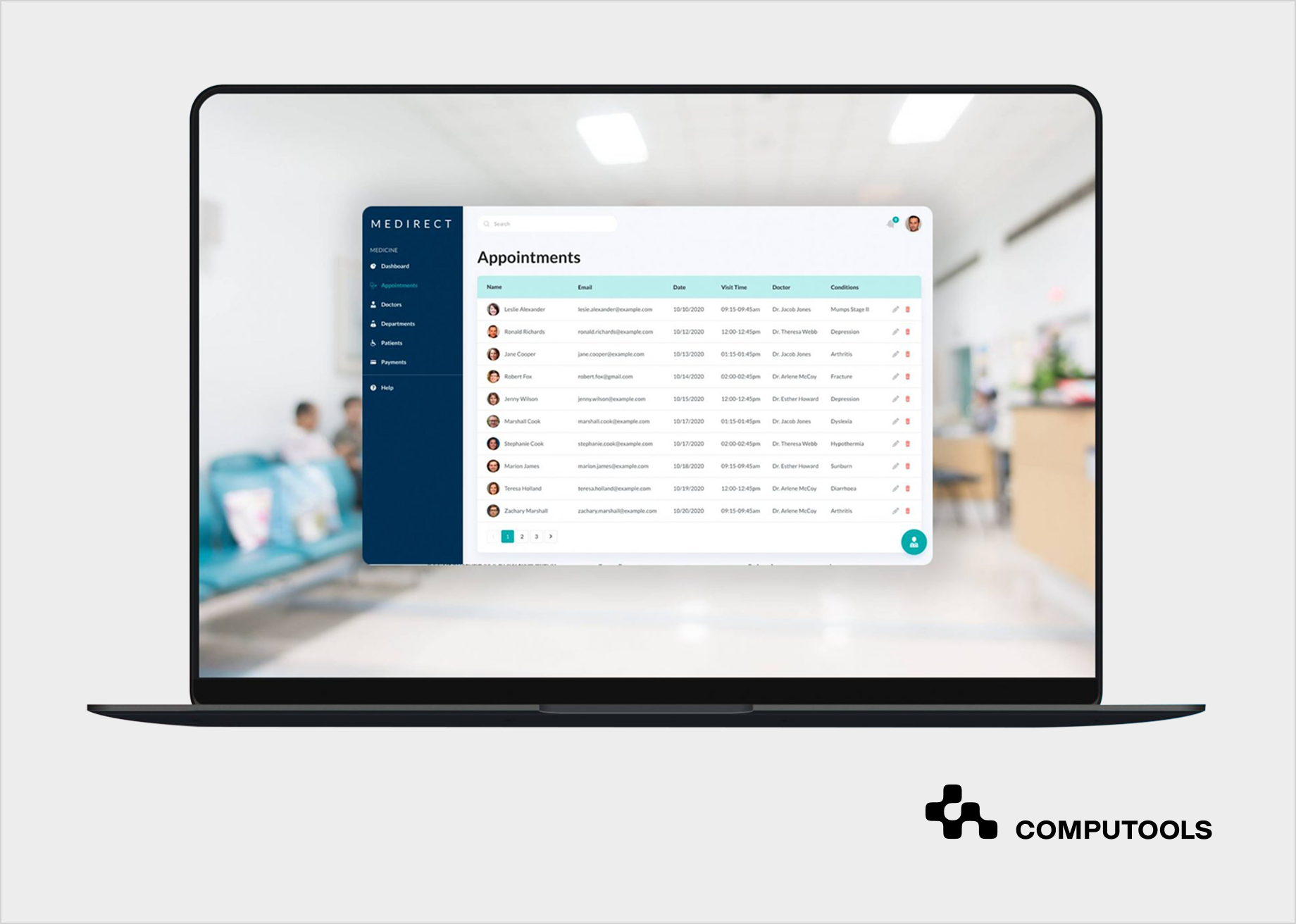
We addressed this challenge while working on Medirect, a healthcare startup focused on improving operational efficiency across healthcare facilities.
The goal was to create a centralized foundation for clinical documentation, unifying patient records and role-based workflows while enabling intelligent data analysis, drawing on our experience delivering AI development services for complex healthcare environments.
The core challenge lay in fragmented data sources and inconsistent calculation logic across local systems. Patient metrics were stored in different formats, processed separately, and often required manual reconciliation. This fragmentation made it difficult to access complete patient histories and limited the feasibility of scalable clinical charting software development within existing workflows.
To solve this, we designed and implemented a centralized platform that standardized medical data and documentation workflows, providing a secure and scalable architecture ready for AI-driven clinical documentation and decision support.
Key outcomes of the Medirect project included:
• Centralized access to patient records and medical histories across facilities
• Consistent data models and standardized calculation logic across systems
• Reduced manual documentation effort and reconciliation overhead
• Improved diagnostic accuracy enabled by complete patient visibility
• A scalable architectural foundation ready for AI-enabled clinical documentation
Following the platform’s launch, Medirect increased its market share by 15%, validating the business value of a unified documentation foundation.
In the next section, we break down the practical steps hospitals can follow to design a production-ready AI clinical documentation and charting system.
Step-by-step: how to build an AI clinical documentation and charting system for hospitals
Building an AI clinical documentation system means designing a workflow-aware, secure, and auditable pipeline that fits how clinicians actually work. Based on real-world implementations, including the Medirect project, the process typically unfolds as follows.
Step 1: Design the healthcare documentation workflow before automation
Every hospital already has a documentation workflow, whether it is explicit or not. The first step is to make it visible, measurable, and intentional. This means mapping how clinical information moves from patient intake through consultations, diagnostics, discharge, and follow-up.
Hospitals should identify:
• where documentation is created versus finalized;
• which roles contribute at each stage;
• where delays, rework, or data loss occur.
Without a clearly defined healthcare documentation workflow, AI will only accelerate existing inefficiencies. In the Medirect project, unifying fragmented workflows across facilities was essential before introducing any intelligent process automation.
Step 2: Reduce clinician workload with real-time data capture
The biggest productivity gains come from eliminating after-the-fact documentation. This is where medical transcription AI software becomes foundational.
Instead of relying on clinicians to reconstruct encounters hours later, AI captures clinical dialogue and contextual signals directly during the visit. The system runs unobtrusively in the background, listening, structuring, and organizing information without interrupting the clinician–patient interaction. This approach shifts documentation from a retrospective task into a concurrent process aligned with how care is actually delivered.
By producing structured drafts in near real time, the system significantly reduces clinicians’ cognitive load. Important details are less likely to be omitted, inconsistencies are easier to detect, and the gap between care delivery and finalized documentation narrows from hours—or days—to the same clinical shift. This is particularly impactful in high-volume environments, where documentation backlogs directly contribute to burnout and delayed billing.
Currently, the goal is to develop a dependable starting point that transforms blank charts into review-ready content. Clinicians stay in control, reviewing and improving drafts rather than creating notes from scratch. As the system learns documentation patterns and specialty-specific language over time, the quality of initial drafts improves, further decreasing manual effort without losing clinical accountability.
Step 3: Convert captured data into reliable clinical charts
Capturing clinical dialogue is only the first step. Real value emerges when raw inputs are transformed into structured, clinically reliable charts that align with how providers read, validate, and act on documentation.
An AI scribe for hospitals should automatically organize captured information into standardized chart formats such as SOAP (Subjective, Objective, Assessment, Plan) or specialty-specific templates. This includes clearly separating subjective patient input, objective findings, clinical assessment, and care plans while preserving clinical intent and context. Consistent structure reduces ambiguity, improves readability, and makes documentation usable across care teams.

Structured charting also enables downstream processes. When notes follow predictable formats, it becomes easier to support coding accuracy, clinical decision support, quality reporting, and audit readiness. In contrast, loosely structured or narrative-heavy notes increase review time and introduce interpretation risk, especially in multi-provider environments.
In the Medirect project, standardizing how patient data was represented across teams and facilities eliminated inconsistencies that previously complicated analysis and clinical decision-making. By enforcing uniform chart structures, the platform ensured that clinicians could quickly understand patient status regardless of where the data originated, laying a foundation for scalable documentation and future AI-driven enhancements.
At this stage, clinicians must recognize the charts as clinically sound, familiar, and easy to review. When structured documentation feels natural rather than imposed, adoption accelerates and the benefits of AI-assisted charting compound across departments.
Step 4: Build compliance and security into the system core
In clinical documentation, security and compliance determine if a system can be used in production. From the first architectural decisions, an AI documentation platform must be designed as HIPAA compliant clinical software, not adapted to compliance after deployment.
Hospitals must ensure role-based access aligned with clinical responsibilities, secure authentication mechanisms, and immutable audit trails that record every interaction with patient data. Each edit, approval, or correction to a clinical note must be traceable to who made the change, when it occurred, and what the previous state was.
AI introduces additional risk if governance is unclear. Automated drafts, model-assisted edits, and learning loops must be fully transparent and controllable. Clinicians and compliance teams need confidence that AI-generated content does not bypass established review processes or obscure clinical accountability.
In the Medirect project, a security-first approach enabled data centralization without increasing compliance exposure. By embedding access controls and auditability into the platform’s foundation, the system could scale across facilities while preserving trust with medical staff and meeting regulatory expectations.
At this stage, the primary focus shifts from delivery speed to long-term trust, audit readiness, and organizational confidence in the system.
Security and compliance must be addressed from the first architectural decisions. How to Design HIPAA-Compliant HealthTech Architecture From Day One explains how to embed compliance into system design rather than retrofitting it later.
Step 5: Connect AI-generated documentation to hospital EHR systems
AI-generated documentation creates real value only when it becomes part of the official medical record. If notes remain in a parallel system or require manual transfer, automation shifts effort instead of eliminating it. This is why robust hospital EMR/EHR integration solutions are a critical success factor for any AI clinical documentation initiative.
Hospitals must ensure approved clinical notes flow into the EHR without reformatting, duplication, or loss of context. Integration should preserve authorship, timestamps, version history, and approval status, keeping documentation defensible for clinical, billing, and regulatory purposes. The system must adapt to existing workflows, not vice versa.
Poor integration is one of the most common reasons AI documentation projects stall. When clinicians are forced to copy content between systems or manually reconcile discrepancies, adoption drops quickly. Conversely, when AI-generated notes appear in the EHR as familiar, complete entries, trust increases and usage scales organically across departments.
In the Medirect project, centralizing patient data while maintaining flexible integration points allowed the platform to support daily clinical operations without disruption. This approach ensured that documentation enhancements improved efficiency without introducing new operational friction, an essential requirement for hospital-wide deployment.
At this step, success is measured by invisibility. When AI documentation is fully integrated, clinicians experience fewer clicks, faster chart completion, and no additional system complexity. From the hospital’s perspective, this translates into faster reimbursement cycles, cleaner records, and a documentation pipeline that can scale with patient volume.
Step 6: Ensure interoperability through healthcare data standards
Clinical documentation does not exist in isolation. Hospitals operate within complex ecosystems that include EHRs, laboratory systems, imaging platforms, billing tools, analytics environments, and external partners. Without interoperability, AI-generated documentation quickly becomes siloed, limiting its long-term value.
This is where HL7 FHIR integration for EHR becomes essential. By mapping AI-generated outputs to standardized healthcare data models, hospitals ensure that documentation can move reliably across systems without semantic loss. Structured notes, observations, medications, and care plans remain interpretable not only by clinicians but also by downstream systems that depend on consistent data.
Standards-based integration reduces vendor lock-in and future rework. As hospitals expand AI usage from documentation to analytics, decision support, and reporting, FHIR-aligned data structures allow new capabilities to be added without redesigning core infrastructure. This flexibility is especially important as regulatory expectations and interoperability mandates continue to evolve.
In the Medirect project, standardizing how patient data was represented enabled unifying records across facilities while keeping the platform extensible. The same principle applies to AI documentation systems: when interoperability is built in from the start, hospitals gain confidence that today’s automation will not constrain tomorrow’s innovation.
Success now depends on durability. Interoperable documentation keeps AI-generated content usable, auditable, and valuable as systems, partners, and clinical needs evolve.
For organizations planning broader AI adoption beyond documentation, How to Integrate AI Diagnostics Into Existing Hospital Workflows explores how diagnostic AI can be embedded into live clinical processes without disrupting care delivery.
Step 7: Plan for scale, iteration, and long-term evolution
AI documentation systems are dynamic, evolving with clinical workflows, regulations, and automation expectations. Hospitals treating AI documentation as a one-time setup often face limitations within a year. The focus moves from initial rollout to sustained use, requiring planning for onboarding departments, expanding documents, refining templates, and adding AI features without disrupting operations. A design for incremental change is essential instead of large-scale rewrites.
Long-term success also depends on continuous improvement. As clinicians interact with AI-generated drafts, feedback loops help improve accuracy, adapt to specialty-specific language, and reduce review time. Monitoring performance, adoption rates, and exception patterns becomes as important as the initial build.
This stage requires long-term technical stewardship rather than one-time delivery, ensuring the system evolves alongside clinical, regulatory, and organizational change.
In the Medirect project, this approach ensured that the platform remained relevant as usage grew and new requirements emerged without destabilizing the core system.
Success now depends on resilience. A scalable AI documentation platform helps hospitals adapt to growth, regulation, and innovation without restarting implementation, safeguarding investments and clinician trust.
Step 8: Operationalize the system, measure impact, and scale adoption
Once a clinical documentation system is technically deployed, the real work begins. Hospitals must transition from implementation to daily operation, ensuring that the system delivers measurable value across clinical, operational, and financial dimensions.
At this stage, organizations should define clear success metrics, including documentation time per encounter, chart completion latency, clinician adoption rates, after-hours documentation reduction, and downstream effects on billing and compliance. These indicators help distinguish between perceived automation and real operational improvement.
Equally important is structured rollout. Successful hospitals expand adoption in phases, starting with motivated teams or high-burden departments, validating results, and then scaling across specialties and facilities. This controlled expansion builds clinician trust, surfaces workflow gaps early, and prevents disruption at scale.
In the Medirect project, this operational mindset ensured that the platform moved beyond a functional launch into a stable, widely used system. By monitoring usage patterns and iterating based on real clinical behavior, the solution continued to deliver value as scope and complexity increased.
This final step ties the entire approach together. It is the practical answer to how to build clinical documentation software for hospitals with AI, not as a one-time deployment, but as a governed, continuously improving capability embedded into everyday clinical operations.
Building and scaling an AI clinical documentation platform is not only a technical task—it is an organizational change that affects clinicians, compliance, operations, and patient experience. The difference between a successful rollout and a stalled pilot often comes down to execution: workflow alignment, integration depth, governance, and long-term support.
This is where experienced healthtech software development services matter. Teams that understand clinical environments, regulatory constraints, and hospital-scale systems can translate AI capabilities into production-ready solutions that clinicians trust and actually use. With the right partner, AI documentation moves from experimentation to a stable, scalable part of everyday care delivery.

Assess the clinical, security, and interoperability requirements of an AI documentation system. Connect with our experts to scope architecture, timelines, and project cost.
What to expect when you build clinical documentation software with AI
Building AI-powered clinical documentation software delivers tangible benefits for hospitals and health systems, but only when expectations are aligned with reality. Below is a practical breakdown of what organizations gain and the challenges they must address during implementation.
Benefits of AI Clinical Documentation Systems
Faster documentation and reclaimed clinician time
• AI chart generators produce structured notes in seconds.
• Clinicians shift from manual typing to quick review and approval.
• Same-day documentation replaces after-hours charting.
• Automation software for clinical notes greatly decreases “pajama time” and mental effort.
Higher accuracy and documentation consistency
• Reduced transcription errors and missed details.
• Uniform structure across providers and departments.
• Improved clinical clarity for downstream teams.
• AI-assisted drafts become more accurate over time through feedback.
Seamless continuity with existing systems
• AI-generated notes flow directly into EHR documentation software.
• Authorship, timestamps, and version history are preserved.
• No duplicate records or parallel workflows.
• Billing, reporting, and audits benefit from cleaner data.
Real-time documentation during patient encounters
• Medical transcription AI software captures dialogue as care is delivered.
• Notes are created while context is fresh, not reconstructed later.
• Clinicians remain focused on patients rather than on screens.
• Documentation delays are largely eliminated.
These benefits compound when documentation moves from post-visit tasks to real-time clinical support, especially in high-volume hospital environments.
AI scribes as a new documentation baseline
• An AI scribe listens passively during visits.
• Conversations are converted into structured clinical charts.
• Providers review rather than dictate or type.
• Adoption is highest in high-volume and high-burnout departments.
Organization-wide Impact
For healthcare organizations
• Increased patient capacity without extending work hours.
• Lower transcription and administrative costs.
• Better compliance through standardized documentation.
• More structured data for analytics and population health.
For patients
• Faster access to visit summaries.
• Clearer communication and care plans.
• Improved coordination between providers.
Key challenges in AI clinical documentation implementation
| Challenge | How It Shows Up | Why It Becomes a Problem |
| Data quality and fragmentation | Inconsistent, duplicated, or incomplete patient records | Low accuracy of AI outputs, reduced trust, and weak analytics |
| Workflow misalignment and adoption | Extra steps for clinicians, parallel tools, and limited training | Low adoption, minimal productivity gains from clinical notes automation software |
| EHR integration complexity | Legacy systems, partial APIs, custom interfaces | Delayed rollout, higher costs, stalled scaling |
| Compliance and auditability | Poor traceability of edits and approvals | Regulatory risk, billing delays, audit exposure |
| Over-automation of clinical notes | Generic notes lacking clinical nuance | Increased review time, lower clinical value |
| Scaling and long-term evolution | Pilot success without sustainable expansion | Stalled ROI, growing maintenance burden |
Why healthcare providers choose Computools
Computools builds production-grade healthcare software used daily by clinicians and administrators across hospitals, clinics, and healthtech companies in the US, EU, the Middle East, and Asia. For over 12 years, we have delivered systems that directly impact patient care through reliability, security, and performance.
Healthcare providers work with Computools because we design solutions around real clinical workflows rather than forcing teams to adapt to generic platforms. Our approach to custom hospital software development enables modernization without disrupting care delivery or increasing operational risk.
Our teams deliver measurable results in live environments: faster access to patient data, reduced administrative costs through automation, and improved care coordination across fragmented systems. In practice, this translates into quicker clinical decisions, fewer errors caused by inconsistent records, and lower workload for medical staff.
A key differentiator is our experience embedding AI directly into hospital IT ecosystems with governance and auditability in mind. Through AI governance services, we ensure AI-driven systems remain transparent, compliant, and scalable over time, rather than becoming isolated tools that are difficult to maintain.
Our experience is proven in live clinical environments, where AI-powered systems must operate under real workload pressure, strict compliance requirements, and zero tolerance for downtime. Healthcare organizations choose Computools when they need a long-term technology partner, not just a vendor.
If you are evaluating potential technology partners, the Top 25 Healthtech Software Development Companies in 2026 provides an overview of teams with proven experience in delivering regulated, production-ready healthcare systems.
Conclusion
AI is reshaping how clinical documentation is created and managed, but real value comes from systems designed around clinical workflows, interoperability, and regulatory requirements, not from isolated tools.
When implemented correctly, clinical documentation automation reduces administrative burden, improves record quality, and allows clinicians to focus more on patient care. Hospitals benefit from faster documentation cycles, cleaner data, and more reliable downstream processes.
Achieving these outcomes requires a strategic approach. AI clinical documentation system development with HIPAA compliance must combine workflow alignment, secure architecture, clinician trust, and scalability beyond pilot deployments. Organizations that invest in this foundation build documentation systems that support long-term efficiency, compliance, and quality of care.

Computools
Software Solutions
Computools is a digital consulting and software development company that delivers innovative solutions to help businesses unlock tomorrow.








“Computools was selected through an RFP process. They were shortlisted and selected from between 5 other suppliers. Computools has worked thoroughly and timely to solve all security issues and launch as agreed. Their expertise is impressive.”